An ischemic stroke is death of an area of brain tissue (cerebral infarction) resulting from an inadequate supply of blood and oxygen to the brain due to blockage of an artery.
People who have any symptom suggesting an ischemic stroke should go to an emergency department immediately. The earlier the treatment, the better are the chances for recovery. Unfortunately, most patients arriving hospitals miss the therapeutical window which was usually 4-8 hours after artery occlusion, therefore, are not indicated for thrombolysis (the breakdown (lysis) of blood clots by pharmacological means, and commonly called clot busting. ). Other treatments are usually symptomatic or supporting only.
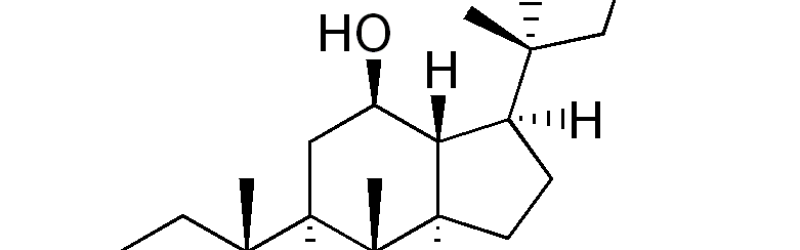
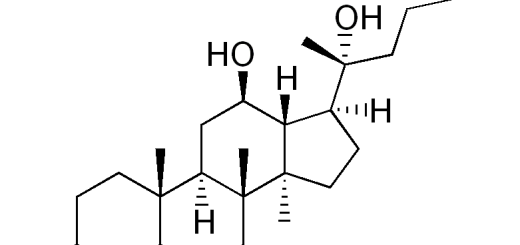
Ginsenosides are major ingredients in ginseng, and are responsible for the majority of pharmacological effects of ginseng. In Asian ginseng, protopanaxatriol-type ginsenosides take the preponderance. These ginsenosides will be metabolized into an aglycone form – protopanaxatriol (PPT), which bears the strongest activity compared to its precursor saponins.
With respect to ischemic stroke, PPT is able to enhance the ability of the brain to resist anoxia sequent to ischemia attack and reduce the infarction size, reported in a Master’s degree research thesis, Zhongshan University, 2006.
In the research, multiple animal models were used to thoroughly assess the PPT role in ischemic stroke.
First, acute anoxia was created in mice by decapitation, and PPT pre-conditioning for 3 days increased the time of gasping breath, suggesting the brain resisted the anoxia better than before.
Then, a localized ischemic stroke was replicated in SD rats by closure of medial cerebral artery after intraperitoneal injection of PPT once for 2 days. Strikingly, the pre-use of PPT improved the hemiplegic signs, reduced the infarction size and brain swelling with alleviation of secondary neuron injury.
Furthermore, PPT was infused intravenously and mean arterial pressure, heart pressure, cerebral blood flow volume and cerebral vessel resistance were measured. The results demonstrated that PPT at doses of 12.3mg/kg、24.6mg/kg and 49.6mg/kg could reduce cerebral vessel resistance within 30 minutes, with accompanying increase in cerebral blood flow volume. PPT injection did not affect heart rate and mean arterial pressure.
Platelets are thought to initiate a series of intricate reactions by adhering to the injured arterial lining, aggregating irreversibly to form a platelet plug, on which the thrombosis (blood clotting) finally develops. In the study, the platelet aggregation and thrombosis were also tested. At the doses of 41.54 mg/kg and 83.08mg/kg, PPT significantly inhibited the platelet aggregation as well as the thrombus weight.
Also, the preventative use of PPT could help maintain the integrity of blood-brain barrier as the penetration of Evans blue (a dye indicator) from peripheral blood into the brain was reduced to a large degree, in a incomplete ischemia mouse model in which two common carotid arteries were closed after 3 days of intraperitoneal PPT injection. The intact blood-brain barrier suggests a less likelihood of brain swelling during ischemic attack.
The re-openning of the occluded artery could cause further damage to already injuried tissue, this phenomenon is called ischemia-reperfusion injury. The study also evaulated the PPT effect on this type of injury. A mock reperfusion injury was created in Mongolian gerbil, and PPT was given 24hours after blood reperfusion. The results demonstrated that medium or high doses of PPT could reduced the reperfusion injury, partially due to reduced free radicals by antioxidant SOD.
Taken together, the preventative use of PPT can increase the brain blood flow and the brain ability to resist anoxia, implying a prolonged therapeutical window for thrombolysis and more patients will receive the benefits of thrombolysis. Furthermore, the PPT pre-use reduces the permeability of blood-brain barrier, the infarction size and reperfusion injury, suggesting a better recovery and functional restoration from ischemia stroke.